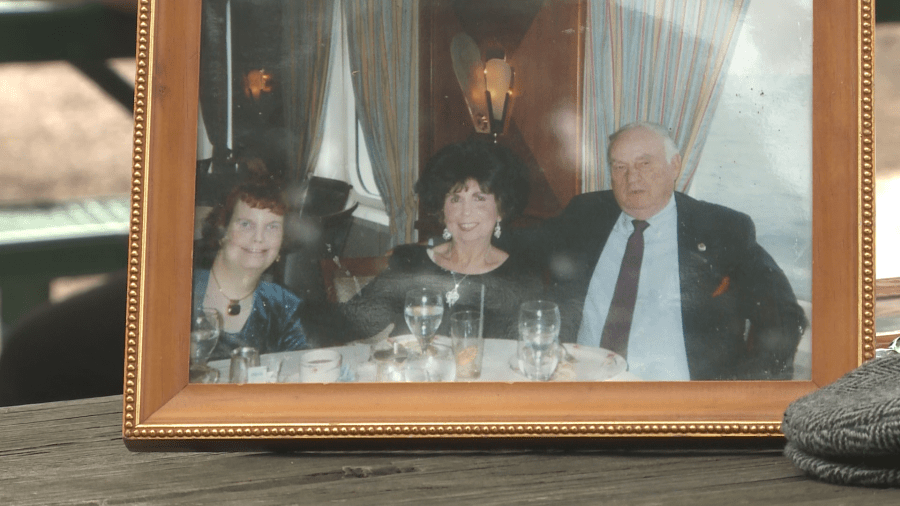
Tina Gansman’s father, 85-year-old Bob Lessel, passed away in August.
He was one of nearly 140 people to die from COVID-19 at long-term care facilities in Shelby County.
“I think that’s the most heart wrenching thing, because I feel like he got snatched from us,” said Gansman.

The statistics are often what people see and hear, but what the numbers don’t show are the people lost, and completely unaccounted are the loved ones left behind.
“My dad was an absolute wonderful, wonderful man. Family man, loved us with all his heart. I have one sister and she’s older than me. And then my mother. They’ve been married for 59 years. He has three grandchildren and a great on the way that he didn’t even get to know about,” Gansman said.
Lessel was buried in his favorite tan hat, and with the ultrasound picture of the great-grandchild to be, he wouldn’t live to meet.
“He taught me that family was everything,”Gansman said. “So, the ultimate family man who taught us what family is. He died alone.”
Lessel was a resident at Quail Ridge Assisted Living and Memory Care.

“One minute we think everything’s fine. The next minute he’s going to the hospital with COVID and then he dies from it. It’s just something, is lacking somewhere,” Gansman said.
Gansman showed WREG letters Quail Ridge’s parent company sent her mother. The first was dated April 29, 2020.
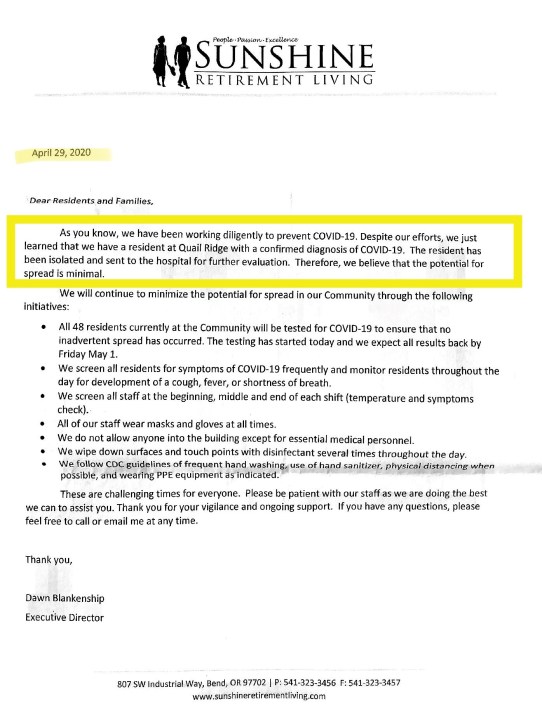
The letter stated, “…we have a resident at Quail Ridge with a confirmed diagnosis of COVID-19.” It further stated the person was isolated and hospitalized, “Therefore, we believe that the potential for spread is minimal.”
However, the virus did spread at Quail Ridge, ultimately to 39 of the 48 residents. Twelve died.
“It took time to reach that point. We never got a phone call and I provided you with a letter that she got, and it said ‘a’ confirmed diagnosis,” explained Gansman.
That same phrase, “a confirmed diagnosis of COVID-19,” shows up again, in a letter dated July 20.
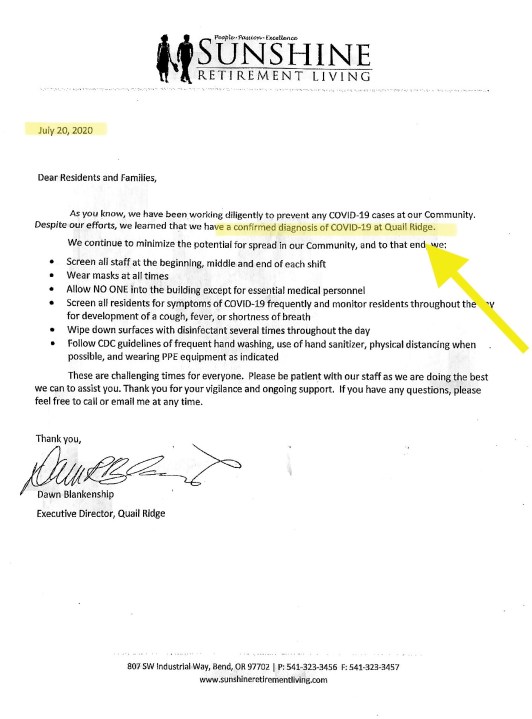
Gansman said her mother received the letter four days later, on July 24. That was the same day Lessel was rushed to the hospital, and a day after the local health department said the cluster was identified at Quail Ridge.
Gansman told WREG, “Please keep in mind that my mom was calling every couple of days to check on him. ‘He’s fine. Everything’s good here, there’s nothing going on.’ But there was.”
WREG reached out to Quail Ridge and we were directed to a spokesperson working on behalf of Sunshine Retirement Living.

After refusing our interview requests, a spokesperson emailed a statement, saying the facility implemented “strict infection prevention measures,” even going beyond CDC requirements.
The company also listed a timeline of actions, including how the facility communicated with families.
A follow up email read, “…Every authorized representative of Mr. Lessel was spoken to in a timely fashion.”
The WREG Investigators asked officials from the Shelby County Health Department about facility communication with families.
“Well, the communication back to family members is one of the things that’s on the checklist from the CDC tool, and it’s one of the responsibilities of the facility,” explained David Sweat, Chief of Epidemiology for the Shelby County Health Department.
WREG asked, “And how do you all determine if that is, in fact happening as it should?”
Sweat replied, “We don’t audit it, we talk to them about it and we make sure that they are aware of their responsibility to do that.”
Responsibility at long-term care facilities is something the WREG investigators have questioned local, state and federal leaders about since the very first outbreak back in March.
We wanted to find out who was going into the facilities when an outbreak occurred, and what they were looking for once inside.
Where your loved one lives determines both the care they receive and the level of oversight the facility faces.
Oversight of nursing homes starts at the federal level, with the Centers for Medicare and Medicaid Services and continues with state survey agencies. In Tennessee, that’s the Tennessee Department of Health.
In the spring, when CMS suspended visitation at nursing homes, they also stopped sending in surveyors for most inspections.
Inspections at nursing homes have since resumed, but with a COVID focus. In addition, for several months during the pandemic, testing in Tennessee was mandatory at nursing homes and reimbursed by the government.
However, such inspections aren’t mandated at places like assisted living facilities and group homes, regulated by various state agencies.
For example, in Tennessee, regulatory authority for assisted living falls under the Department of Health, while many group homes in Shelby County are regulated by the Department of Intellectual and Developmental Disabilities.
WREG asked a spokesperson from the Department of Health if the agency was specifically conducting COVID-Focused Inspections (or any additional inspections) at places like assisted living facilities and we received the following response:
“Federal guidance regarding Focused Infection Control surveys are specific to nursing homes. There is currently no mandated FIC surveys for ACLFs. Health infection preventionists have been working closely with facilities, including assisted care living facilities.”
So we’ve learned, the first line of defense at any long-term care facility with an outbreak, is the Shelby County Health Department.
When there’s an outbreak at a long term care facility, they send in a team of workers, using a special check list, to review practices ranging from infection control to testing compliance.
The team will also often make recommendations.
The report workers use is called an Infection Prevention and Control Assessment Tool
for Nursing Homes Preparing for COVID-19.
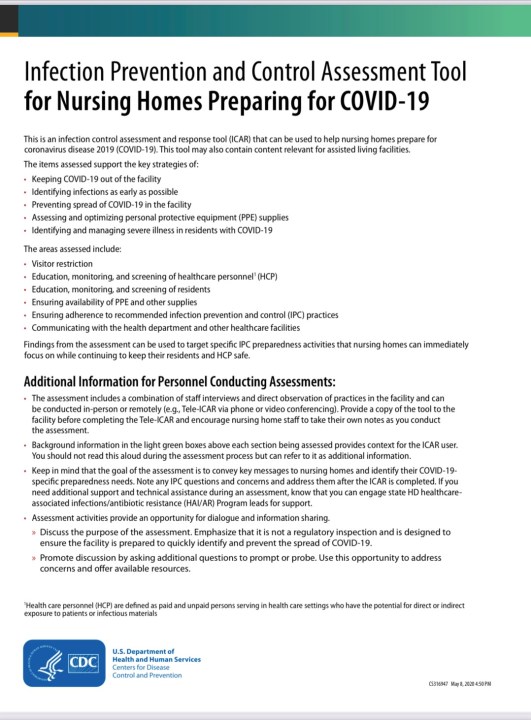
Assessment areas are listed as follows:
- Keeping COVID-19 out of the facility
- Identifying infections as early as possible
- Preventing spread of COVID-19 in the facility
- Assessing and optimizing PPE supplies
- Identifying and managing severe illness in residents with COVID-19
“The purpose of the tool is for us to check and see what are the practices in place, where could there be some improvements,” explained Sweat.
WREG has reviewed assessments dating back to March for dozens of area long-term care facilities.
Records reveal just how unprepared some places were at the start of the pandemic with critical shortages of PPE and nurses.
Some didn’t stop visitation or admissions soon enough and weren’t screening residents and staffers as recommended.
The health department visited Quail Ridge twice, once in late June when investigators found the facility was still having communal dining and residents weren’t wearing masks and staying in their rooms. The documents reveal administrators told the team from the SCHD it was “impossible to keep from groups” and that residents “do what they want due to memory loss”… and related to wearing masks outside rooms they said it’s “impossible with the memory deficits that patients have.”
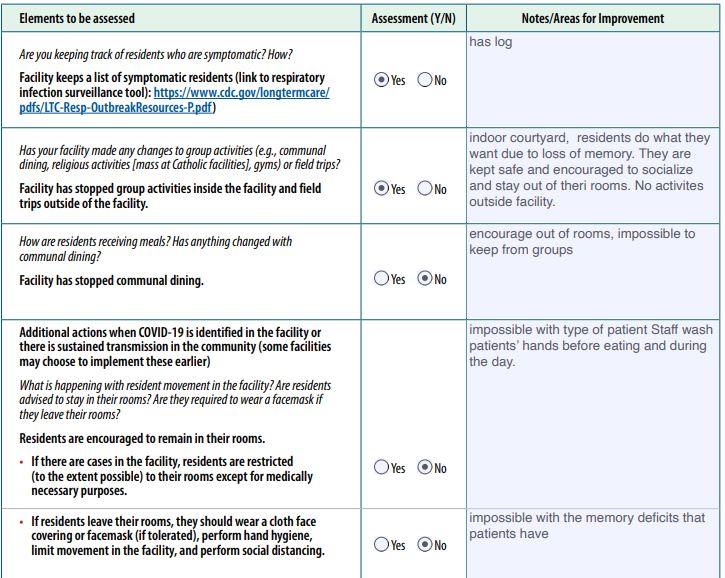
During an August visit, nearly a month after the outbreak turned deadly, the health department asked the facility to come up with an action plan and recommended they change their practice of re-using N-95 masks. The report also revealed the facility asked for help with acquiring masks and gowns because their supplies were “critically low at this time.”



“I know for a fact that something has fallen here. And I know we’re not the only families that this has happened to,” said Gansman.
NewsChannel 3 received emails from Gansman and Sherryl Carlock the very same day.
Carlock’s aunt, 71-year-old Shirley Gatewood, died of COVID-19 in mid-September.
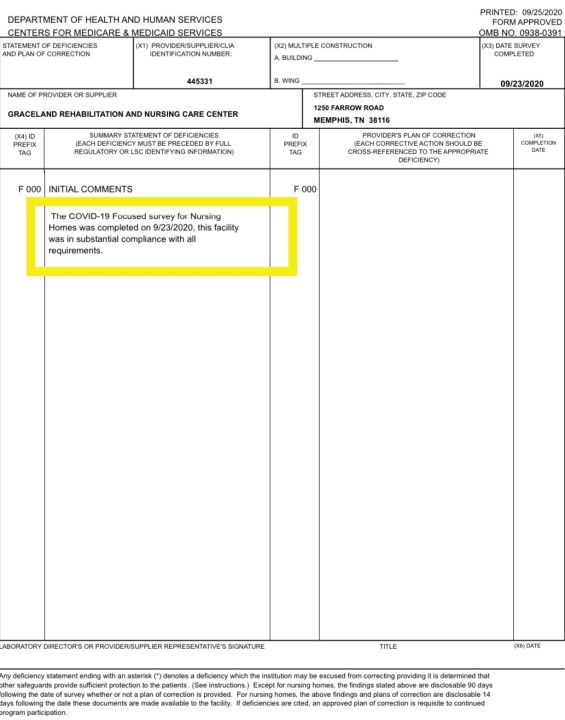
She was a resident at Graceland Rehabilitation and Nursing Center. A recent WREG investigation found that facility has one of largest and deadliest outbreaks in the county, where more than 80 percent of residents were infected.
Two different facilities, two different families with the exact same message.
“We thought she would be protected, in that they stopped any visitation from family members or any outside people other than staff,” said Carlock.
Gansman said, “We felt that he was safe there. In fact, my mom and I had talked about it several times and felt comfort in knowing that he was there and that nothing was being brought in because the visitors had stopped. So we thought he was safe there, but we were wrong.”
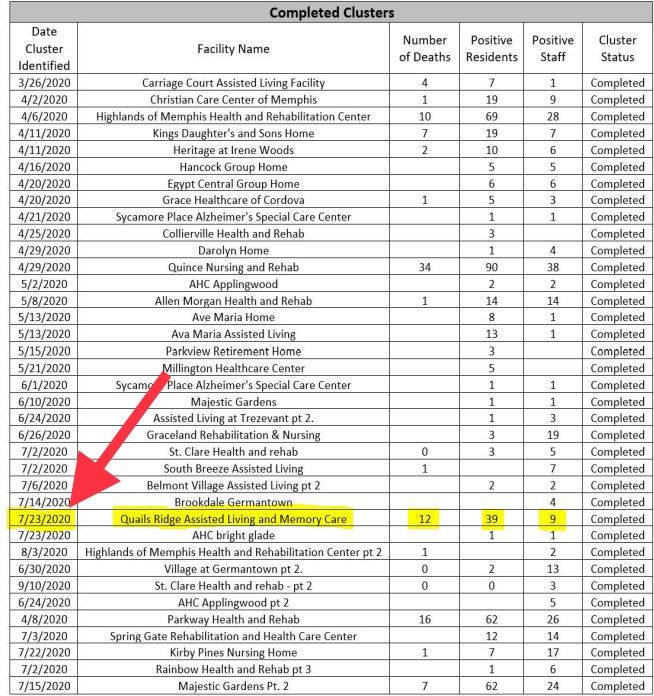
Quail Ridge’s 12 fatalities makes the outbreak the fourth deadliest of long-term care facilities in Shelby County. Only the following facilities had more deaths:
- Quince Nursing and Rehabilitation: 34
- Graceland Rehabilitation and Nursing Center: 19
- Parkway Health and Rehabilitation Center: 16
Both families told WREG they thought their loved ones were protected.
Our reporting has found, even with state and federal oversight, records reveal, facilities with deadly outbreaks are still determined to be in compliance with regulations.
For example, our investigation of Graceland Rehabilitation and Nursing Center showed state regulators visited the one-star nursing home three times since August for COVID-19 Focused Inspection Surveys, along with complaint investigations.
However, each time, surveyors found the facility in compliance.
Also, on a number of assessment tools completed by the local health department, facilities with large outbreaks still received marks of “yes” in numerous categories.
WREG asked Sweat, “So if you’re seeing these ‘Yes’ check marks from the health department and, you know, state department, I’m reading these, they’re saying ‘in compliance’. These families say to themselves, we’re following the rules. She literally said, ‘We didn’t go in.’ But he’s still gone. How do you respond to that? What do you say to that?”
“Yeah, I am so sorry,” said Sweat, who became emotional when talking about it.
“Everyone in this community involved is trying to do their very best, to stop the spread of this. But when, in one of those instances when it occurs, and it leads to a fatality, all we can say is, we honestly did try, to prevent this from happening and we are so sorry,” Sweat said.
“Families should be furious,” said Brian Lee, who runs the advocacy group Families for Better Care.
The former long-term care ombudsman says part of the problem in general, is a historical reliance on self-reporting in the nursing home and long-term care industry.
“It’s a little easy sometimes for facilities to maybe misrepresent the data, kind of mislead the public, the American public. And it’s happened for years. So it wouldn’t be surprising to me if it’s reported one way, but something else is happening entirely different,” explained Lee.
Gansman told WREG, “I’m not sure what policies need to be changed, but there’s no reason, he had a whole family.”

There have been more than 50 COVID-19 clusters at long-term care facilities across Shelby County since the start of the pandemic. There are currently 16 active clusters. The cluster at Quail Ridge was closed in September.
The Shelby County Health Department notes it considers a cluster “resolved” once a facility has gone 28 days without a new case.
Resources for families at long-term care facilities:
Tennessee Long Term Care Ombudsman
Nursing home violations, including recent COVID-19 Focused Inspection Surveys, can be found at the following federal and state websites.
You can search for licensure and violation history at group homes here.
A Centers for Medicare and Medicaid Services spokesperson provided the following response on inspections during the pandemic:
Due to the COVID-19 pandemic, CMS announced changes to the inspection process on March 4 and March 23, to allow inspectors to focus on the most serious health and safety threats like infectious diseases and abuse during the pandemic. CMS’s network of state and federal surveyors conducted infection control surveys at all 315, or 100 percent, of CMS certified nursing homes in Tennessee. We have made these reports available on Nursing Home Compare to keep the public informed. The majority of the inspections of the nursing homes found no deficiencies at the time of the survey. It is important to note that the surveys are conducted at a point-in-time and the presence of COVID-19 in a nursing home, while necessitating a strong infection control response, does not necessarily mean the facility is out of compliance with CMS requirements.