MEMPHIS, Tenn. — Graceland Rehabilitation and Nursing Center, a Whitehaven nursing home that’s been cited for abuse and neglect, is in the midst of one of the largest and deadliest COVID-19 outbreaks among long-term care facilities in Shelby County.
WREG reviewed local, state and federal records and pressed leaders, in search of answers for families who turned to News Channel 3, saying they feel like their loved ones were left unprotected.
Shirley Gatewood was constantly surrounded by family and friends, but it was the close eye she kept on everyone else that earned her the nickname, “The Scout.”
“She watched over everything,” said Gatewood’s niece Sherryl Carlock.
But it was Gatewood who needed the support.
Having lived 71 years with Down syndrome, by many standards, Shirley Gatewood spent her life defying the odds, so it’s the way she died that’s left her family in disbelief.
An emotional Carlock told WREG, “She didn’t have to go like this.”
Gatewood died on Sept. 17, exactly two weeks after being sent to the hospital from Graceland Rehabilitation and Nursing Center.
“They did not let us know that she had COVID,” Carlock said.
“No one is allowed to come in. So then that means you’re going to pick up the response. You’re gonna pick up that additional responsibility to make sure that the loved ones are taken care of,” Carlock said. “And they didn’t.”
Carlock said that despite constant attempts to keep tabs on her aunt’s condition, Graceland didn’t reach out to the family until Gatewood was en route to the hospital on Sept. 3. Carlock said her mother had been receiving robocalls from the facility since the start of the pandemic, painting quite a different picture.
“My mother, who is 86, she was receiving weekly calls from the robocall saying, no, no, no cases, no positive cases or anything like that,” said Carlock.
Then Carlock said, “We received a call on 9/3 that she was being she had been admitted to the Methodist South for evaluation. Of course, you know, we were frantic because she can’t speak for herself and no one was allowed in at the hospitals.”
Carlock said she called back to get a report on her aunt and was told that she came in very ill. A doctor told her Gatewood had a UTI, was dehydrated, was septic, had low blood pressure and low potassium.
Carlock says the following day, doctors confirmed Gatewood’s positive COVID diagnosis.
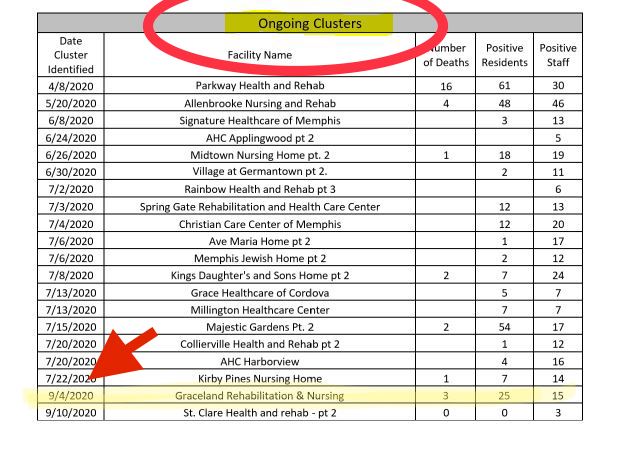
That same day, Sept. 4, is the date officials with the Shelby County Health Department say a new coronavirus cluster was identified at Graceland.
It’s the second outbreak there this year, and has infected eight out of 10 residents at the facility.
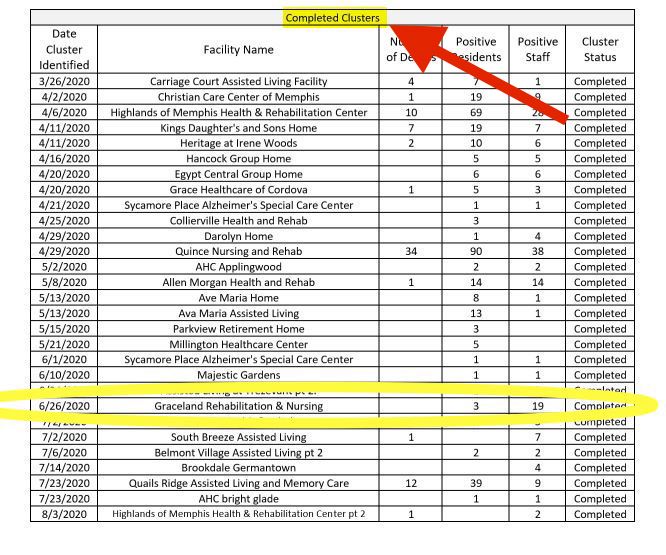
Graceland’s first outbreak was in late June. Three residents and 19 workers tested positive.
“That facility clearly has had some issues for a while, and it looks like they had been improving, but then we have a new cluster in the place,” said David Sweat, chief of Epidemiology with the Shelby County health Department.
It was a cluster that was apparently already spreading, as the health department considered the first one closed.
Take a look at the photos below. Each day, the SCHD releases an update on COVID-19 cases, including clusters at long-term care facilities. WREG has been tracking and saving the data.
During the week of Sept. 7 (first photo taken on 9/8), Graceland’s first cluster appeared on the “Ongoing Clusters” list.
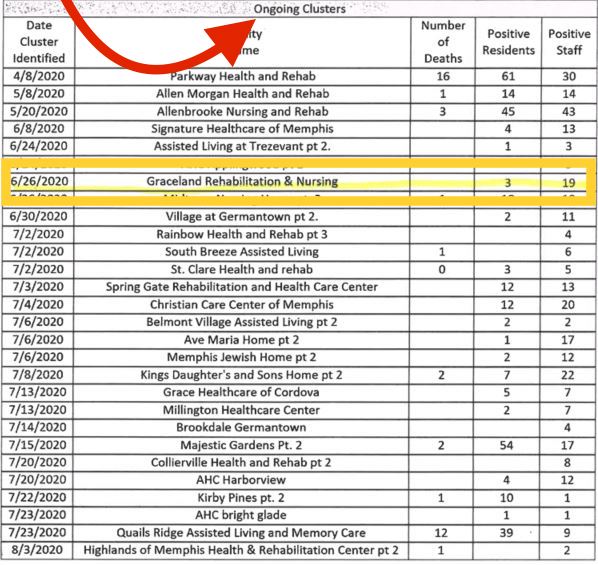
Days later, over the weekend, it moved to the “Completed Clusters” list.
Then, by the following week, (picture below taken on 9/14) a new cluster with a date of September 4th appeared on the “Ongoing Clusters” list.
By mid-September, the facility went from three deaths to five, and in a single day (Sept. 14 to 15), resident cases more than doubled. As the days went by, the case count continued to climb. By the end of September, there were 114 positive cases at Graceland.

WREG asked Sweat, “How does that happen and how do they even get removed from the completed list?”
According to the Shelby County Health Department, a cluster is considered resolved once a facility has gone 28 days without a new case. But subsequent testing may have revealed a new cluster.
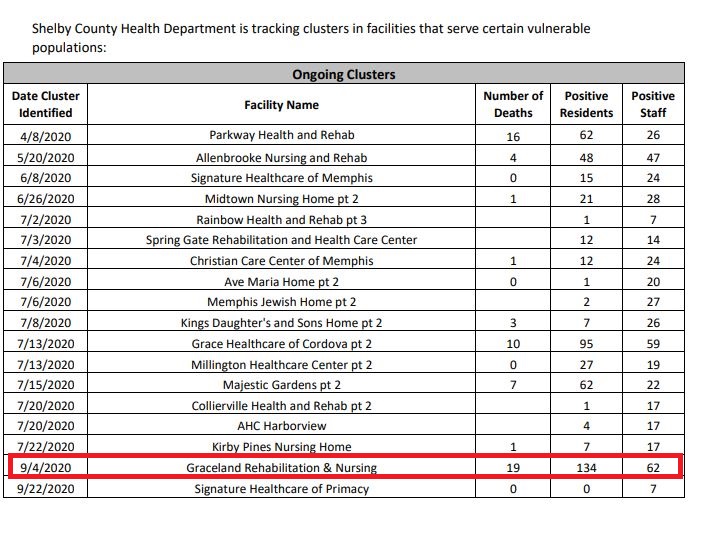
By late October, 19 residents of Graceland Rehabilitation and Nursing had died from coronavirus.
Sixty-two staff members tested positive, along with 134 residents. Records show that in June, there were 157 residents at Graceland. That means more than 80% of the seniors living there were infected at some point.
Graceland’s had the largest outbreak and the second deadliest of long-term care facilities in the county.
As WREG shared the data with Carlock, she said, “Something is not right.”
“What what needs to be done to prevent this? You know what, what are we doing?” she asked.
WREG learned federal regulators just put Graceland on a potential watch list for nursing homes with a pattern of serious problems. They’re called Special Focus Facilities and Graceland is now a candidate for that list. Graceland has been on the candidate SFF list for two months.
Graceland is not currently on SFF list. However, according to state regulators, facilities that do become Special Focus Facilities are surveyed twice a year for regulatory compliance for a period of 18 months. During that time period, the facilities must demonstrate they can come into compliance, or risk termination from the Medicare/Medicaid program.
Records show state regulators, who never agreed to our multiple interview requests, visited Graceland three times since August for COVID-19 Focused Inspection Surveys, along with complaint investigations.
However, each time, surveyors found the facility in compliance.
Carlock asked, “How can they be in compliance?”
The WREG Investigators also obtained records from the Shelby County Health Department documenting its visits at Graceland Rehabilitation and Nursing Center.
A team from the SCHD visited Graceland on July 23 after the first cluster was identified. Investigators from SCHD’s Infection Prevention Control team visited again on Sept. 8 and 28, with a notation for a re-visit on Oct. 5.
The report from the Sept. 8 visit reveals the nursing home was still setting up its COVID unit as of Sept. 4. That’s the same day the outbreak was identified.
The report goes on to detail that the facility conducted “mass testing” on 9/2/20, which resulted in 17 cases.
The same September report reveals officials from the health department called Graceland’s administrator to “see if they were ok,” The report notes the administrator “stated mass testing uncovered a lot of cases.” That call came after “news coverage,” according to the records, with the health department offering more help. The administrator admitted to “continued challenges” with staffing, education and other issues.
The visit also uncovered some additional problems at the facility as noted below.
During that visit, the team from the health department made several recommendations including:
- Ensure COVID Designated area has proper signage “Boldly” presented
- Work closely with the SDPH on prevention measures for COVID reduction
- Create a dedicated team to care for COVID patients with independent equipment for each resident
Dorothy McClinton emailed WREG in early October, saying her 76-year-old mother Rubbie Hordges, also a resident at Graceland, tested positive for the virus in October.
Prior to that positive test, McClinton says her mother’s roommate tested positive, but she tested negative twice, and the family requested isolation and a room change.
“What they did, instead of quarantine her for 14 days, my mother, because she had been in a with a positive patient, they moved her in a room with another negative lady for 14 days. So now my mom, I got a call Thursday that my mom is positive,” McClinton said.
That was the first week in October. McClinton also told WREG she had trouble getting answers from the facility.
“Oh, my God! By Saturday morning my mama called my sister and told my sister she had been in her room ever since 7 that morning, she was in feces and she was soaking wet. She had not been cleaned up that day at all,” a teary McClinton said.
The families we spoke with weren’t alone. WREG reached out to Graceland’s administrator several times, and failed to get a response.
Eventually, Graceland’s administrator Machelle Calaway emailed a statement.
Calaway said a portion of the facility is designated “for the isolation of potential or suspected cases.”
She also said employees are tested weekly and must report any work outside Graceland. In addition, she said the facility communicates “openly and often” with residents and their loved ones.
“All I can say is, Graceland, you got to do a better job, Shelby County Health Department, you’ve got to do a better job,” Carlock said. “State government, you got to do a better job to protect those that can’t protect themselves.”
After a brief hospitalization, McClinton says mother is doing much better, and so is Graceland regarding communication. However, she says she was initially kept in the loop by people on the inside at Graceland. One of those workers told WREG mass testing wasn’t done until September, and residents had already died.
“I promise you, if she ever can get a negative test, I’m bringing her home with me,” cried McClinton.
Communication with families regarding COVID-19 cases at long-term care facilities is required by CDC guidelines.
WREG asked officials from the Shelby County Health Department about McClinton’s complaint regarding her mother not being re-located to another room.
Officials said in an emailed response to followup questions, “The facility has to have a bed available and conducive to the family’s needs, staff is allocated for the bed/private room request overall the ability to grant the family’s request, and the patient census should allow for a bed request or swap to occur.”
The SCHD also said Graceland Rehabilitation and Nursing Center had three zones set up for patients with a “broad spectrum” of exposures.
History of Violations
Graceland Rehabilitation and Nursing Center is a one-star facility, the lowest possible rating from federal regulators.
The facility has faced numerous fines by both state and federal regulators in the past.
Most recently, the Centers for Medicare and Medicaid Service fined the facility $183,305 for violations based on a complaint investigation conducted in February of 2020.
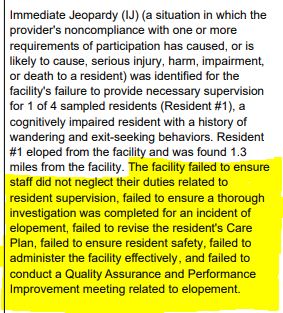
It was cited with what’s called Immediate Jeopardy (the most serious type of violation) for health citations related to Substandard Quality of Care.
In January, a resident in a wheelchair left the facility by getting out through a window, then a hole in the fence. Federal documents show the resident crossed a major, seven lane highway and walked to a neighborhood more than a mile away.
Surveyors noted the facility didn’t know she was missing until a police officer brought her back nearly three hours later. This came after a resident called 911 because a “suspicious female” was knocking on doors of houses in the area.
The report noted the following:
“The facility neglected to ensure a safe environment and neglected to adequately supervise…a cognitively impaired resident…”
The nursing home was also fined more than $7000 for violations during a visit in October of 2019. The facility’s last regular survey was conducted in July of 2019 and it was cited with 13 violations.
Also in July of 2019, The Tennessee Department of Health fined Graceland Rehabilitation and Nursing Center $250 for a survey conducted in June where surveyors found medication wasn’t stored properly.
A Centers for Medicare and Medicaid Services spokesperson provided the following response on inspections during the pandemic:
Due to the COVID-19 pandemic, CMS announced changes to the inspection process on March 4 and March 23, to allow inspectors to focus on the most serious health and safety threats like infectious diseases and abuse during the pandemic. CMS’s network of state and federal surveyors conducted infection control surveys at all 315, or 100 percent, of CMS certified nursing homes in Tennessee. We have made these reports available on Nursing Home Compare to keep the public informed. The majority of the inspections of the nursing homes found no deficiencies at the time of the survey. It is important to note that the surveys are conducted at a point-in-time and the presence of COVID-19 in a nursing home, while necessitating a strong infection control response, does not necessarily mean the facility is out of compliance with CMS requirements.


















